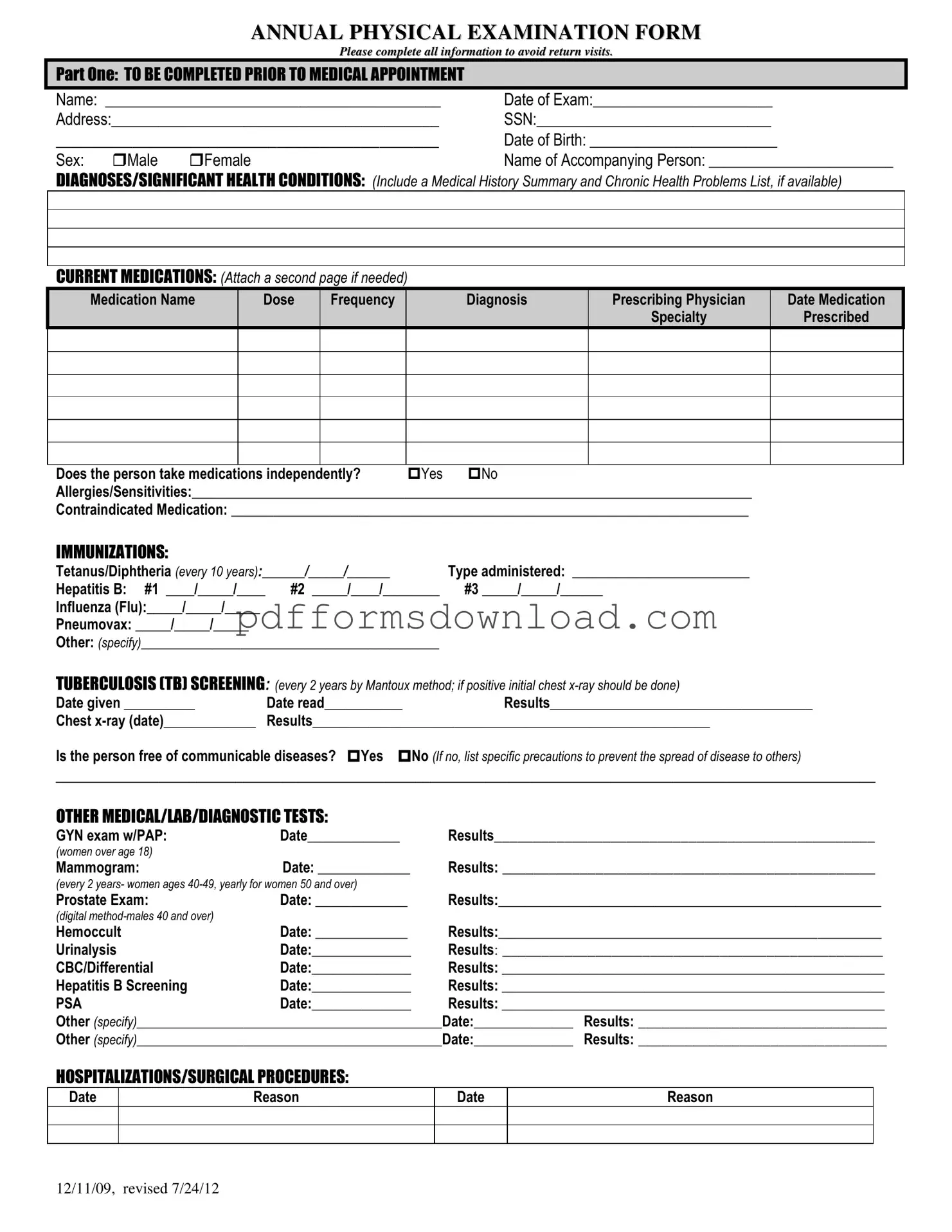
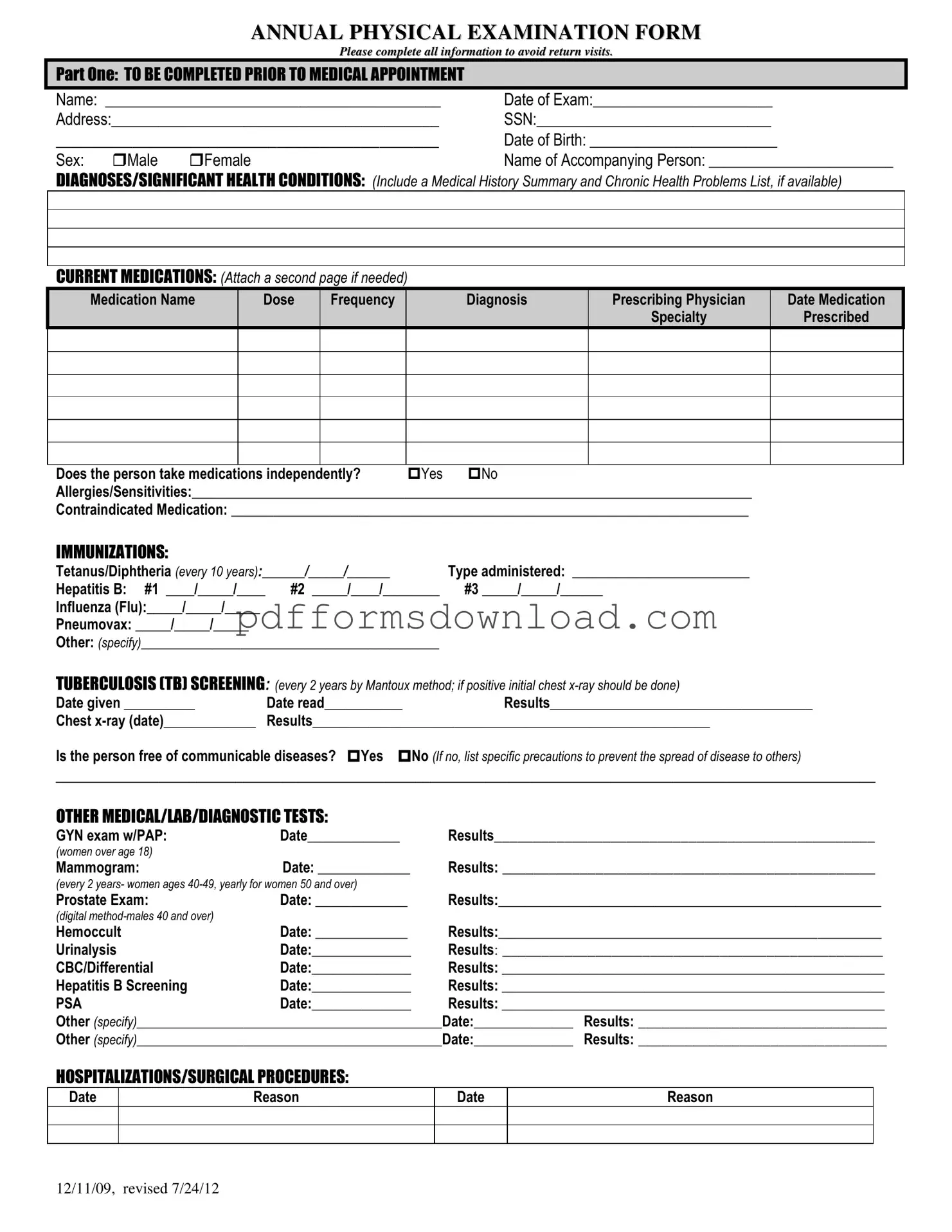
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to gather comprehensive health information about an individual prior to their medical appointment. This information helps healthcare providers assess a patient’s overall health, identify any significant medical conditions, and recommend appropriate screenings or treatments. Completing the form thoroughly can help avoid the need for return visits due to missing information.
What information is required in Part One of the form?
Part One requires basic personal details, including the patient's name, date of birth, and address. It also asks for a summary of medical history, current medications, allergies, and immunization records. This section is crucial for understanding the patient’s health background and ensuring safe and effective care.
How should I list my current medications on the form?
When listing current medications, include the medication name, dosage, frequency, the diagnosis for which it was prescribed, and the prescribing physician's information. If you take multiple medications, you can attach an additional page to ensure all medications are documented clearly.
What should I do if I have allergies or sensitivities?
If you have allergies or sensitivities, it's important to list them in the designated section of the form. This information helps healthcare providers avoid prescribing medications that could cause adverse reactions and ensures your safety during treatment.
Why is tuberculosis (TB) screening included in the form?
TB screening is included because it is a common requirement for many healthcare assessments, particularly in settings where communicable diseases may pose a risk. The form prompts for TB screening every two years, and if the test is positive, a follow-up chest x-ray is necessary to rule out active TB disease.
What types of additional medical tests are mentioned in the form?
The form mentions several additional tests, including GYN exams with PAP smears, mammograms, prostate exams, and various lab tests such as urinalysis and complete blood counts. These tests are recommended based on age and gender, helping to identify potential health issues early.
What happens if I have had recent hospitalizations or surgical procedures?
Recent hospitalizations or surgical procedures should be documented in the specified section. Providing this information allows healthcare providers to understand your medical history better and consider any complications or ongoing treatments that may affect your current health status.
How can I prepare for the physical examination?
To prepare for the physical examination, ensure that you complete the form accurately and bring any relevant medical records. It’s also helpful to write down any questions or concerns you may have regarding your health, as this can facilitate a more productive discussion with your healthcare provider.
What should I do if my health status has changed since my last examination?
If your health status has changed, you should indicate this on the form and specify the changes. This information is vital for your healthcare provider to tailor your examination and any necessary treatments or recommendations based on your current health needs.
Who should I contact if I have questions about filling out the form?
If you have questions while filling out the form, it’s best to contact your healthcare provider’s office. They can provide guidance and clarify any sections that may be confusing, ensuring that you complete the form accurately and comprehensively.