What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) or other life-saving measures in the event of cardiac arrest or respiratory failure. This order is typically used by individuals with terminal illnesses, severe health conditions, or those who wish to avoid aggressive medical interventions at the end of life.
Who can request a DNR Order?
Generally, a DNR Order can be requested by any competent adult. This includes patients who understand their medical condition and the implications of the order. In cases where a patient is unable to make decisions, a legally authorized representative, such as a family member or a designated healthcare proxy, may request a DNR on their behalf.
How do I obtain a DNR Order?
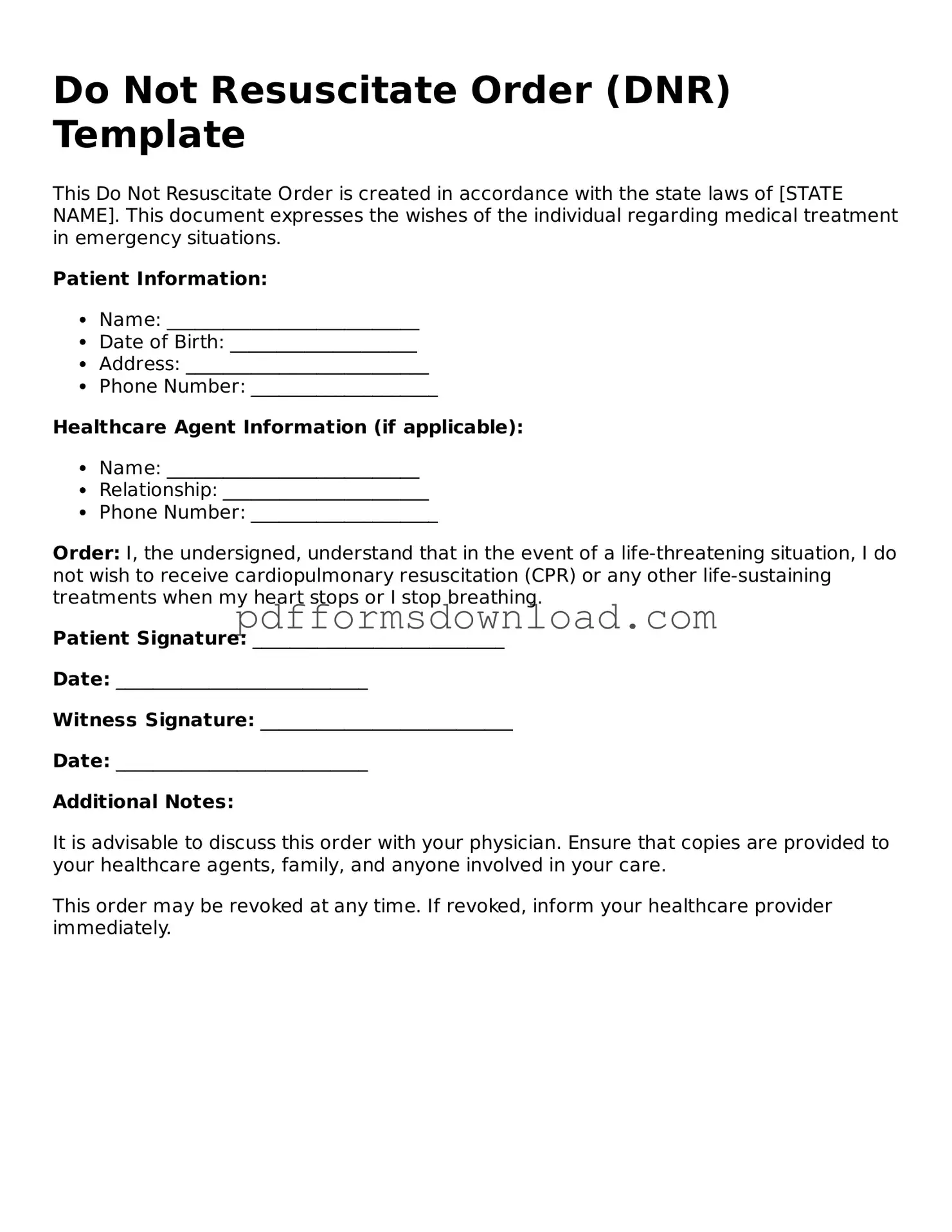
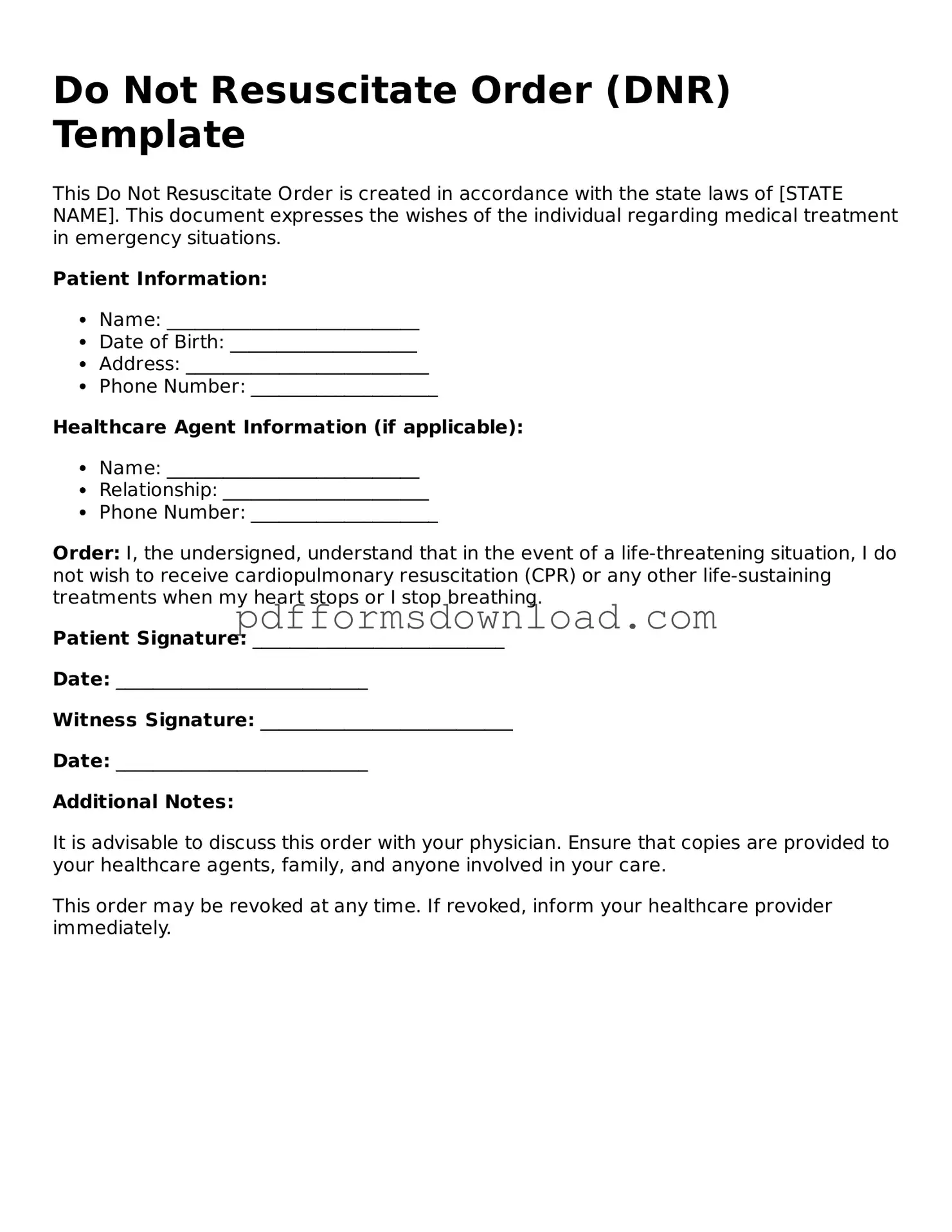
To obtain a DNR Order, you typically need to discuss your wishes with your healthcare provider. They can provide you with the necessary forms and help you understand the implications of the order. Once completed, the DNR must be signed by both you and your physician to be valid. It's essential to keep copies of the signed order in accessible locations, such as with your medical records or at home.
Will a DNR Order affect other medical treatments?
No, a DNR Order specifically addresses resuscitation efforts. It does not prevent you from receiving other medical treatments or interventions. Healthcare providers will continue to offer appropriate care, such as pain management and comfort measures, even if a DNR is in place.
Can I change or revoke my DNR Order?
Yes, you can change or revoke your DNR Order at any time. If you decide to modify your wishes, simply inform your healthcare provider and complete a new DNR form. Make sure to distribute the updated order to all relevant parties, including family members and healthcare providers, to ensure your wishes are respected.
What happens if I am admitted to a hospital with a DNR Order?
If you arrive at a hospital with a DNR Order, the medical staff will review your order and respect your wishes. They will focus on providing comfort and appropriate care according to your preferences. It’s important to communicate your DNR status to the hospital staff upon admission to ensure that your wishes are honored throughout your stay.
Are DNR Orders recognized in all states?
Yes, DNR Orders are generally recognized across all states, but the specific laws and regulations governing them can vary. Some states have specific forms that must be used, while others allow for more flexibility. It’s crucial to familiarize yourself with the laws in your state to ensure that your DNR Order is valid and will be honored by healthcare providers.