What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet (MARS) is designed to track and document the administration of medications to consumers. It ensures that medications are given at the correct times and allows healthcare providers to monitor adherence, effectiveness, and any potential side effects.
Who should use the Medication Administration Record Sheet?
This form is intended for use by healthcare professionals, caregivers, and facilities responsible for administering medications to individuals. It is essential for anyone involved in medication management to maintain accurate records for compliance and safety.
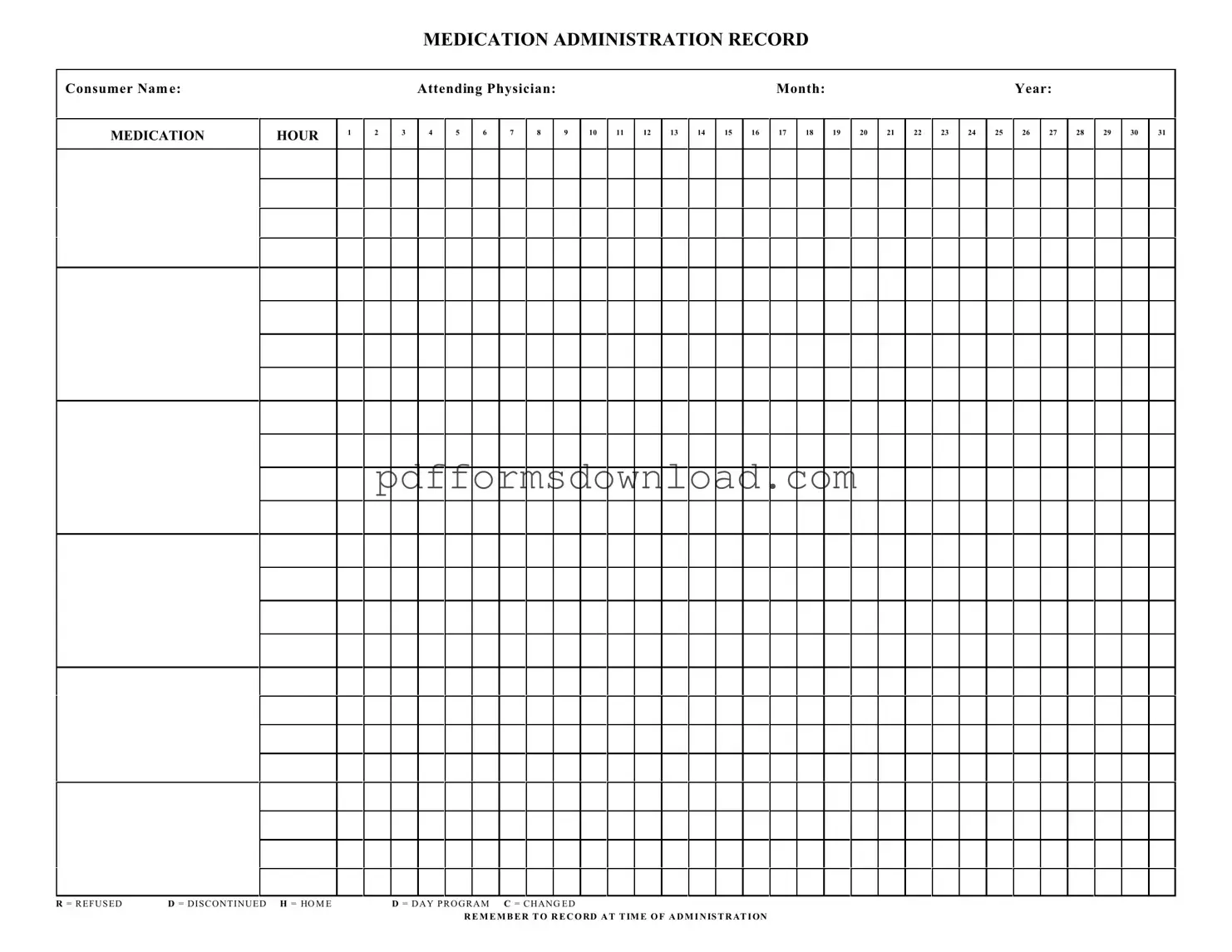
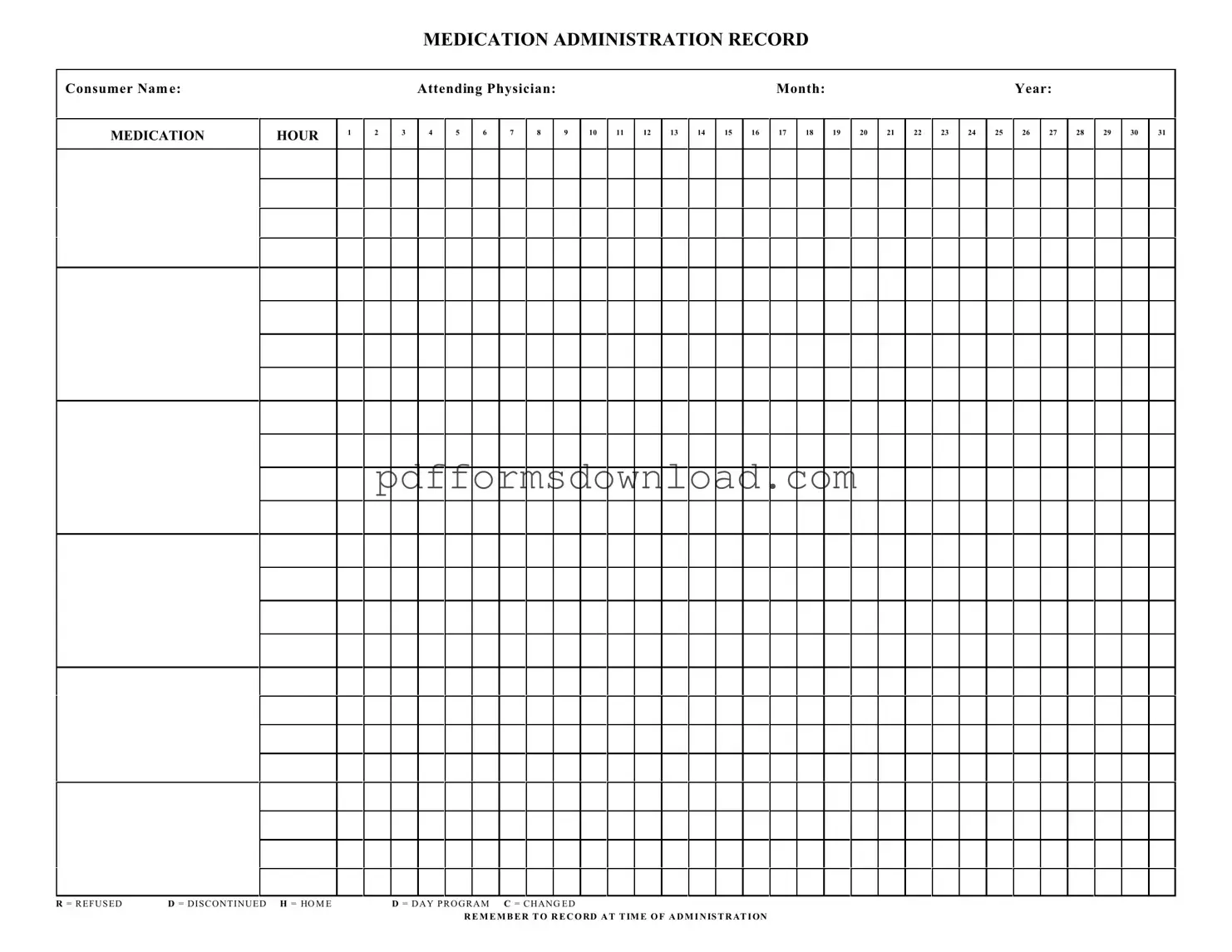
What information is required on the Medication Administration Record Sheet?
The MARS requires the consumer's name, the attending physician's name, and the month and year for which the medications are being administered. Additionally, it includes spaces for recording each medication's administration times and any relevant notes regarding refusals or changes in medication.
How do I record medication administration on the form?
When administering medication, mark the appropriate hour on the form. If a medication is refused, discontinued, or changed, use the designated codes: R for refused, D for discontinued, H for home, D for day program, and C for changed. It's crucial to record this information at the time of administration to ensure accuracy.
What should I do if a medication is refused?
If a consumer refuses medication, it must be documented on the MARS by marking the corresponding hour with an "R." Additionally, note any reasons for refusal, as this information is vital for ongoing care and communication with the healthcare team.
Can the Medication Administration Record Sheet be used for multiple consumers?
No, the MARS is specific to individual consumers. Each consumer should have their own record sheet to maintain clear and accurate documentation. This practice helps prevent errors and ensures that each consumer's medication regimen is monitored effectively.
How often should the Medication Administration Record Sheet be updated?
The MARS should be updated daily or whenever medications are administered. Consistent and timely updates are essential for maintaining an accurate record of a consumer's medication history and for ensuring compliance with prescribed treatment plans.
What are the consequences of not properly documenting medication administration?
Failure to document medication administration can lead to serious consequences, including medication errors, adverse health effects, and legal liability. Accurate records are essential for ensuring consumer safety, effective treatment, and compliance with regulatory requirements.