What is the purpose of the TB Test form?
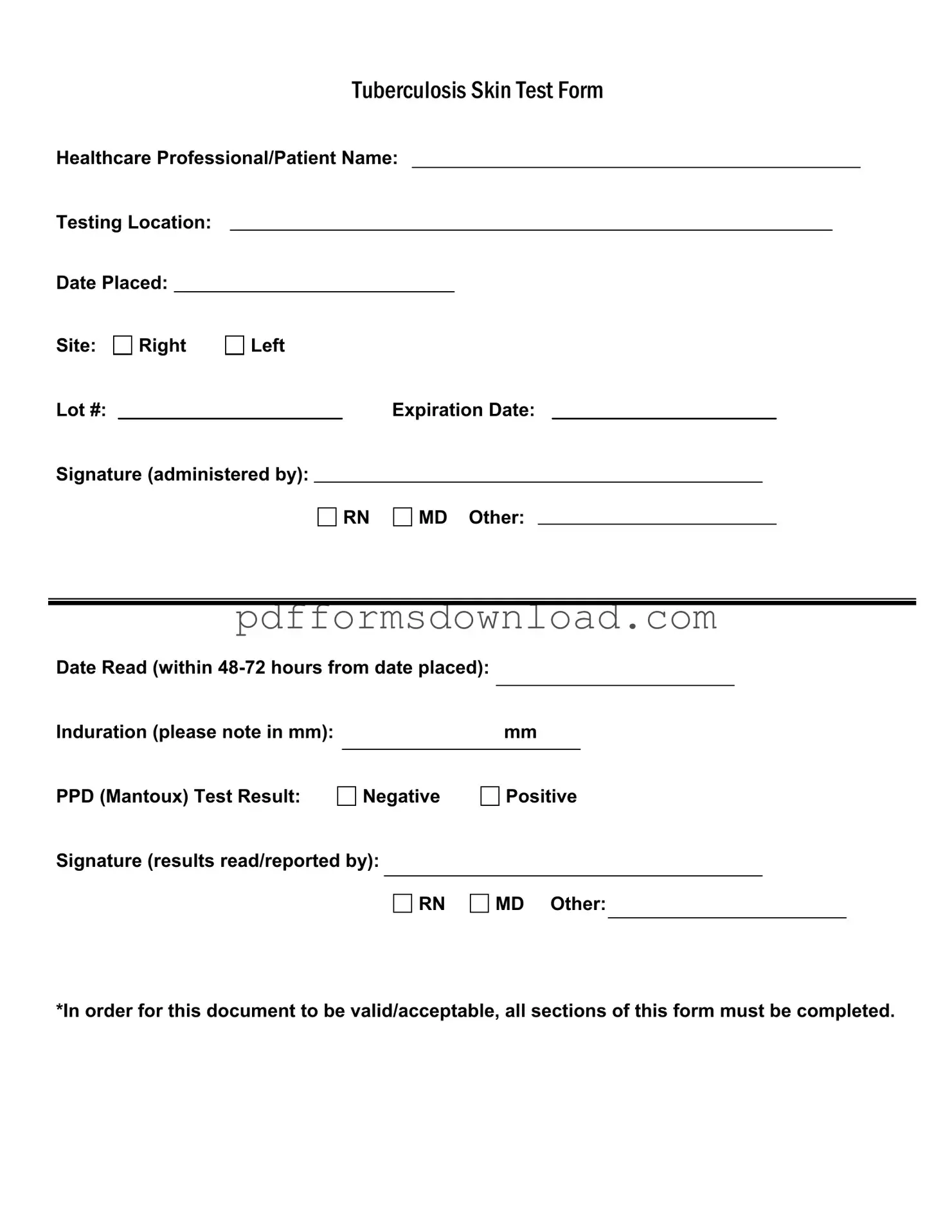
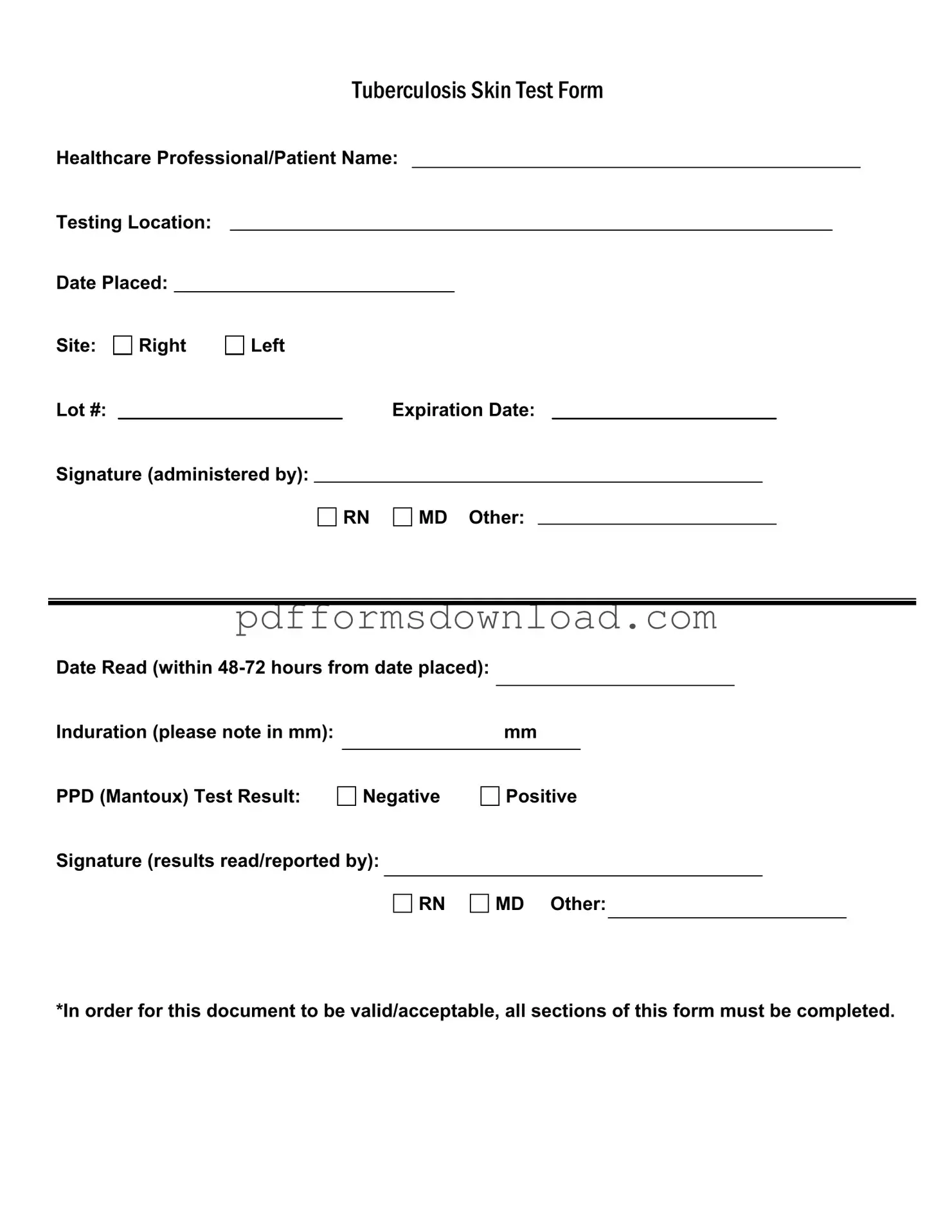
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. It ensures that all necessary information is recorded for both healthcare professionals and patients, allowing for accurate tracking of TB screening results.
Who needs to fill out the TB Test form?
This form must be filled out by a healthcare professional who administers the TB test. Additionally, the patient’s information should be included to maintain accurate records. This ensures that both parties have a clear understanding of the test results and any necessary follow-up actions.
What information is required on the TB Test form?
Essential information includes the names of the healthcare professional and patient, the testing location, the date the test was placed, the site of administration (right or left arm), lot number, expiration date, and signatures of the administering and reporting healthcare professionals. Induration measurement and the test result (negative or positive) must also be documented.
How soon should the results be read?
The results of the TB test should be read within 48 to 72 hours from the date it was placed. This timeframe is crucial for accurate interpretation of the test results, as the induration measurement may change if not read within this period.
What does the induration measurement indicate?
Induration is the raised, hardened area that forms at the test site. The measurement is taken in millimeters (mm) and indicates the body’s immune response to the TB antigens. A larger induration may suggest a positive test result, but interpretation can vary based on individual risk factors and health history.
What does a positive TB test result mean?
A positive TB test result indicates that the individual has been exposed to the TB bacteria and may have an infection. However, it does not confirm active TB disease. Further evaluation, including a chest X-ray or additional tests, may be necessary to determine if the individual has active TB.
What should be done if the TB test result is negative?
A negative result typically means that the individual has not been infected with the TB bacteria. However, if there are symptoms or risk factors present, further testing may be recommended. Always consult with a healthcare professional for personalized advice.
Can the TB Test form be used for other purposes?
This form is specifically designed for documenting the TB skin test. It is not valid for other types of medical tests or procedures. For other health screenings, separate forms should be utilized to ensure proper documentation.
What happens if the TB Test form is incomplete?
For the TB Test form to be valid and acceptable, all sections must be completed. An incomplete form may lead to confusion or misinterpretation of the test results, potentially impacting patient care. It is essential to ensure that every required field is filled out accurately.
Who is responsible for signing the TB Test form?
The form must be signed by the healthcare professional who administered the test and the one who read the results. This ensures accountability and provides a clear record of who performed and interpreted the test.