What is a Do Not Resuscitate (DNR) Order in Washington State?
A Do Not Resuscitate Order is a medical order that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a patient's heart stops beating or if they stop breathing. In Washington State, a DNR order is a legal document that reflects a patient's wishes regarding resuscitation efforts during a medical emergency.
Who can request a DNR Order?
In Washington, any competent adult can request a DNR order. This includes individuals who understand the implications of the order and can communicate their wishes. Additionally, a parent or legal guardian can request a DNR order for a minor. In cases where a patient cannot make their own decisions, a legally authorized representative may also be involved.
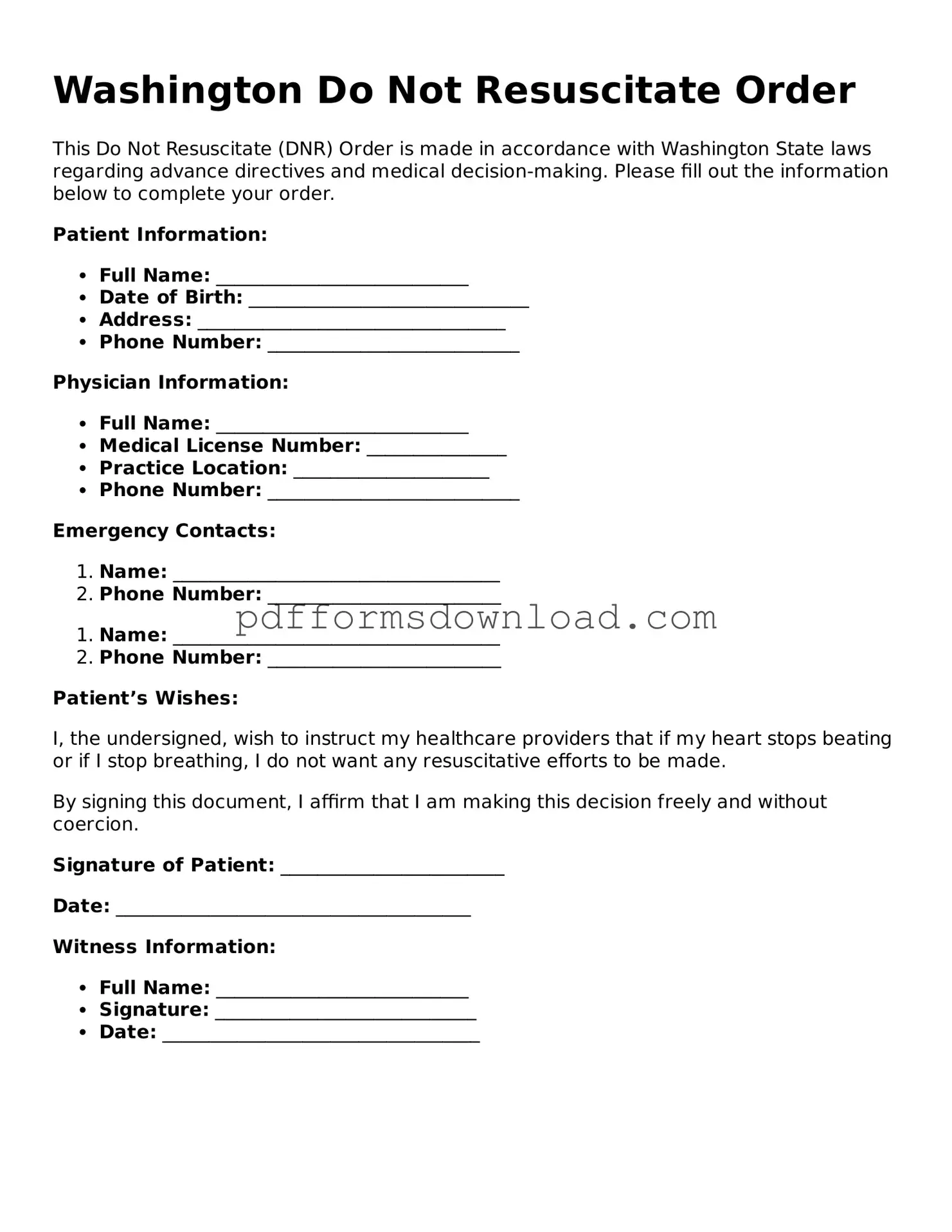
How do I obtain a DNR Order in Washington State?
To obtain a DNR order, a patient must discuss their wishes with a healthcare provider. This conversation often takes place during a routine medical appointment or when a serious illness is diagnosed. If the healthcare provider agrees that a DNR order is appropriate, they will complete the necessary paperwork. It is essential for patients to ensure that the order is properly documented and filed in their medical records.
Is a DNR Order the same as an Advance Directive?
No, a DNR order is not the same as an advance directive, although they are related. An advance directive is a broader legal document that outlines a person's preferences for medical treatment and decision-making in the event they become incapacitated. A DNR order specifically addresses resuscitation efforts. Patients can include a DNR order as part of their advance directive, but they are distinct documents.
What happens if a DNR Order is not honored?
If a DNR order is not honored, it can lead to unwanted medical interventions that go against the patient's wishes. In Washington, healthcare providers are legally obligated to respect a valid DNR order. If a DNR order is not followed, patients or their families may have grounds for a complaint or legal action against the healthcare provider or facility.
Can I change or revoke my DNR Order?
Yes, a DNR order can be changed or revoked at any time. A patient must communicate their decision to their healthcare provider, who will then update the medical records accordingly. It is crucial to ensure that any changes are documented to avoid confusion during a medical emergency.
Where should I keep my DNR Order?
Patients should keep their DNR order in a location that is easily accessible to both themselves and their healthcare providers. Many people choose to keep a copy in their medical records, at home, or with a trusted family member. It is also advisable to wear a medical alert bracelet or carry a card that indicates the existence of a DNR order.
Does a DNR Order apply in all medical situations?
A DNR order specifically applies to situations involving cardiac arrest or respiratory failure. It does not prevent healthcare providers from offering other forms of medical treatment or care. Patients will still receive necessary medical interventions for other health issues, such as pain management or comfort care, even with a DNR order in place.
How does a DNR Order affect my family?
A DNR order can relieve family members of the burden of making difficult decisions during a medical crisis. By clearly expressing their wishes, patients can help ensure that their loved ones do not have to struggle with the decision to pursue or forgo resuscitation efforts. However, it is essential for families to discuss the order openly to avoid misunderstandings.
Can a DNR Order be used in all healthcare settings?
Yes, a DNR order is valid in all healthcare settings, including hospitals, nursing homes, and at home. However, it is important for patients to ensure that their DNR order is communicated effectively to all healthcare providers involved in their care. This helps ensure that their wishes are honored, regardless of where they receive treatment.